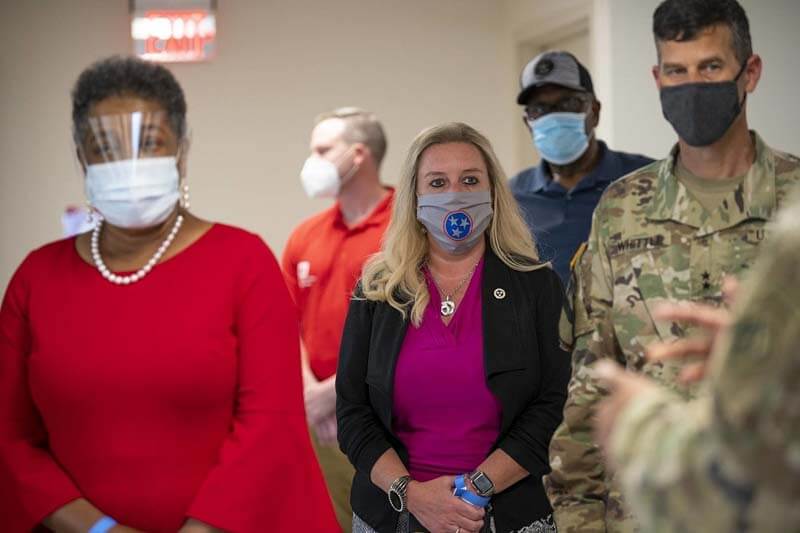
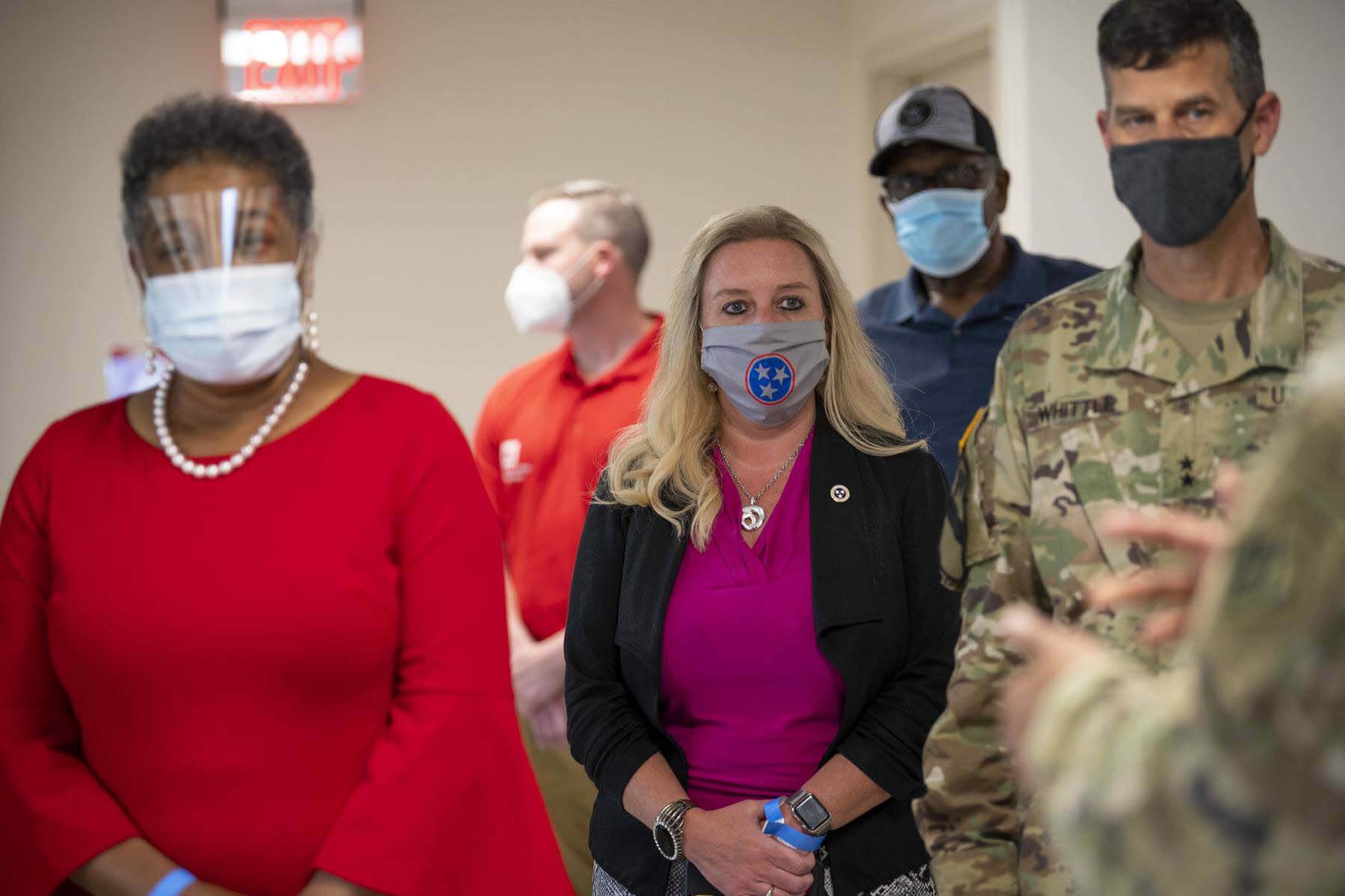
By now, you’ve likely been affected by COVID-19 in one way or another. Many of us have experienced fears of exposure, wondered if we should voluntarily self-quarantine, or thought twice about a headache that wouldn’t otherwise faze us. Despite an endless stream of available information on the news and internet, you may still have nagging questions — and if so, you’re not alone. From defining what “close contact” means, to explaining when to get tested after suspected exposure, Dr. Lisa Piercey, Commissioner of the Tennessee Department of Health, answered our most burning COVID-19-related questions (that pertain to everyone, not “just” Tennesseans!).

Alright, let’s dive right in. What does “close contact” really mean?
“Close contact” means less than 6 feet for 10 minutes or more.
So, if you run into somebody at the park or greenway and you talk to them for three minutes, whether you’re wearing a mask or not, that is not considered “close contact”?
That’s right. If you walk past somebody at the check-in desk, or stand at the water cooler for a couple of minutes and chat while you heat your lunch, that doesn’t count. The more common ways of close contact are sitting in a business meeting with someone, being around the table eating with someone, being in a car with someone, or hanging out at a party for a while and talking. Certainly, if there’s a scenario where you have a lot of voices or singing, those are even higher risk scenarios — such as in a bar. You have to get really close and talk loud because the music is loud and it’s hard to hear. Most people are standing up or sitting in close proximity, and they don’t have the spacing they do at a table. Anytime you have those scenarios of talking, singing, cheering or chanting, those are even higher risk activities because the respiratory droplets propel further than they would in normal talking.
If someone has had a suspected or known exposure, how soon after that exposure should they be tested?
You don’t need to be tested at all if you have been exposed. You just need to quarantine for 14 days. The only reason to be tested after exposure is if you become symptomatic. If you’re exposed, you have to quarantine for 14 days, whether you’re symptomatic or not. Then, if you become symptomatic, you should be tested. But if you remain asymptomatic, you stay in quarantine for 14 days, and then you’re good to go. People want to know how long it’s going to take to show up if they were exposed so they can go get tested, and then if they get a negative test, they think, “OK, I’m cool. I’ve averted that crisis.” That’s not true at all because it might take up to 14 days to show up. So you need to quarantine for that whole time. Once you’ve passed that point, you can go on about your business.
If you DO test positive, you must isolate yourself for 10 days. Does that begin from the day of testing, or the day test results are received?
It’s 10 days from the day of testing. The virus doesn’t care how long it takes the lab to get your results back. The virus is still doing what it does in your body, whether your test results come back tomorrow or eight days from now, so that period starts from the time of your test collection. There’s no way to prove or disprove what day [of the virus] you’re on. When you’re asymptomatic, you’re just as likely to be on the first day as you are to be on the last day unless you have a very clear source of exposure. But because we’re never going to know where you are in that disease process, out of caution, you have to assume you’re at the beginning of it, so you don’t inadvertently spread the virus by getting out too soon.
What does a 14-day quarantine really mean? Can I go to the grocery store with a mask on or take a walk, or am I not allowed to leave my home?
True quarantine is being in your house and not coming into contact with any other humans. Everybody’s situation is a little bit different as far as going outside. It doesn’t mean that you have to stay within the four walls of your home, but if there’s any possibility at all that you’re going to be in contact with another human, then you shouldn’t take a chance. That includes going to the grocery store or picking up takeout. Depending on where you live, you can possibly take a walk outside or sit outside your house. That’s fine. But if you live downtown, and you’re going to come into contact with neighbors or people on the street, or if you’re in a subdivision and you think your neighbors are going to come over and talk to you, then you shouldn’t do that. It’s really lack of human contact for 14 days. I realize that’s strict and stringent. Most people live with other people, so it’s a little bit trickier. Some people don’t have the ability to be in a spare bedroom on the other end of the house. You just need as little human contact as possible.
RELATED: 5 Easy Ways to Boost Your Immune System
Are isolation and quarantine the same thing?
A lot of people use the terms interchangeably, but we need to make a distinction between them. Quarantine is what you do when you’ve been exposed, but you don’t have the illness. Isolation is what you do when you have the virus and test positive. If you’re sick or test positive, even if you’re asymptomatic, that’s an isolation period. You can actually be released from isolation sooner than quarantine if you’re in contact [with someone who’s infected]. Once you’ve had the virus, we know that you can safely resume activities about 10 days after you test positive and have been asymptomatic for at least 24 hours. However, that’s on the back end, after you test positive and isolate for 10 days.
Quarantine is different. It’s on the front end. Quarantine is a full 14 days because that’s how long the virus can take in some people to show up. It’s usually shorter than that, but in some people, it can take that long. So, it’s very likely and common that cases who were exposed quarantine longer than those in isolation.
If you’re with somebody who’s sick, your quarantine is 14 days from the date of your last contact. The CDC explicitly says that household contacts often have to stay quarantined longer, sometimes much longer, than the actual COVID case itself. That’s hard for people to understand. You were exposed as recently as the last time you came into contact with the infected household member. If you’re taking care of that person, then your 14-day quarantine starts when they’ve cleared isolation. The CDC says that sometimes it can be 21 days or longer because the caregiver’s quarantine period doesn’t start until that person is considered recovered.

Does “recovery” mean that someone who has tested positive for COVID-19 has a negative test? Or is recovery when their 10-day isolation is up?
It’s when their 10 days are up. You cannot test your way out of quarantine. You cannot say, “I’m seven days in, and I feel well; let me go get a test. If I’m negative, I can stop this quarantine.” That’s not how that works. We don’t even recommend testing during quarantine unless you become symptomatic, and there’s no testing at the end of quarantine or isolation. The CDC recommends against what we call a “test of cure,” which means that at the end of isolation, people want to make sure they’re negative. That’s not an accurate way to use testing, because sometimes people shed the virus for several weeks after they have it.
So, people potentially continue to test positive even after they’ve satisfied their isolation?
Yes. That’s why we do not recommend retesting; it doesn’t tell us anything we didn’t already know. The test will still be positive, but they’re not infectious or contagious — it’s a non-infectious virus. So, there is no need to test at the end of either quarantine or isolation. That’s called using a time-based strategy, which is the top recommendation of the CDC.
Every test has to be ordered by a doctor, and anytime a doctor orders any test, whether it’s a lab test or a CT scan or whatever, you have to ask yourself, “What am I going to do differently? What is the action that this test result is going to cause?” If the answer is, “Well, I just want to know,” then that’s not an appropriate use of a medical test. This is a really key message. Most of the time, people just want peace of mind; it doesn’t cause any action change. Most people outside of physicians were never taught this concept, so they don’t think this way.
It can come across as cold or uncaring or, even worse, that I don’t want people to know. It’s not that. We have to remember that these are medical tests. Peace of mind is important, but that’s not a medical diagnosis or treatment. We know that patients are going to stay positive, particularly the elderly and immunocompromised. There are some reports that they can stay positive for up to 80 days. You hear all these crazy stories of “Oh, I tested positive again four weeks later, and now I have to go back into isolation.” No, you don’t. You’re still shedding the virus because your body is still trying to process it, but it’s not infectious particles.
If someone is exposed for the entirety of someone else’s isolation because they’re caring for that person, even if they’re not sleeping in close quarters, do they still have to start the 14-day self-quarantine at the end of the other person’s 10-day isolation?
You’ve got it. In that scenario, someone might be on lockdown for 21 days or more. That’s a tough pill to swallow because a lot of people don’t have anywhere else to go. Even if they did, they don’t want to, or they can’t because the person who’s ill needs care. That makes it pretty tricky and pretty frustrating for folks in that situation.
How is it that one spouse can test positive and one test negative? Does that mean a positive test is inevitable if they maintain close contact, or are there some people who simply aren’t getting the virus even after exposure?
Just because you’re exposed doesn’t mean you’re inevitably going to get it. There are close household contacts that test negative throughout, even with known close exposure. We don’t really know why that is, but we see that in many disease processes. A stomach bug is very contagious, but if you have a big family in a household, two or three may get it, and it’s pretty unusual for everybody in the house to get it. We just don’t understand why.
What is the correct protocol if someone lives with a healthcare professional who’s exposed to COVID-19 patients?
It’s not terribly different for the person living there, but the person who works in healthcare needs to take extra precautions. They need to shower and change clothing either before they leave the healthcare facility or immediately upon entering the home. Once that person showers and changes clothes, there are really no additional precautions. Because healthcare workers have such a strong emphasis on personal protective equipment (PPE) and handwashing, they often have lower rates of infection because they take such strong measures all day, every day, as part of their job.
RELATED: How to Meal Prep and Eat Healthy During Quarantine
Why does COVID-19 affect people so differently, and is there a way to know how it will affect us in advance?
We now know that about half of people under 40 who get it are asymptomatic — not all, but many, so we have to be careful about not generalizing the entire population. We know that younger, healthier people are much more likely to be asymptomatic. We also know, for unclear reasons, sometimes otherwise perfectly healthy young people get very ill and even die. It’s very uncommon, but there’s not a good way to predict that. We know that people with health conditions, particularly obesity, hypertension, COPD or emphysema, or cardiac disease, are all at a much higher risk of not only becoming symptomatic but having severe disease requiring hospitalization or even intensive care. And we know that after a lot of people have the infection, they have long-term consequences such as breathing problems and cardiac issues. The virus hasn’t been around long enough for us to know how it’s going to affect us years from now, but we do know that after a few months, people are still having problems. So, the whole narrative of Let me just go ahead and get it and get it over with is pretty risky.
I see a lot of people driving alone and wearing masks. Is that doing anything at all?
No, there’s no medical reason to wear a mask when you’re alone, particularly confined in a vehicle. I think some people think that the virus is going to get sucked up into the air conditioning system, and they’re going to breathe it in, but that’s not how it works. It’s passed human to human, so if you’re not around any humans, then you don’t have to wear it.
If masks have a pocket for a filter, should we use one? If so, what kind should we get?
Some masks allow for a filter. Quite frankly, most of them call for a coffee filter — there’s nothing medical or fancy about that. It doesn’t have to be that, it’s just a multi-layered mask, so it doesn’t really matter what the material is. It’s another layer to create an additional barrier for that viral particle. There have been a few studies on different kinds of masks, like the quilted multi-layered kind for cloth masks seem to be more effective than the single-layered. Then you’ve got your surgical masks, which are typically a three-ply mask. Obviously, the big one is the N95, which is reserved for healthcare workers.
When we hear about reports of positive COVID-19 cases, are those numbers referring to positive tests or to people who test positive? In other words, if someone tests twice, and they have two positive tests, is that being counted in the report once or twice?
Great question! There’s an important distinction. When we say cases, we’re talking about people, and they’re only counted once, no matter how many times they test positive. We also report the number of positive tests, which is on our website, but we don’t advertise that number because it really doesn’t mean anything. The number we report is the number of cases, which is the number of people. It’s only counting humans, not tests.
There are rumors about which deaths are counted as COVID-19 deaths. If someone tests positive for COVID-19 but dies from a non-COVID-19-related cause, is that person added to the number of COVID-19 deaths since they also had COVID-19 when they died?
That’s taken out of the equation. The only deaths that are counted are COVID-related deaths. We’ve had people who we know have COVID who have been in a car wreck and unfortunately died. It’s not counted because COVID did not cause their death. The car wreck caused their death.
And just because it makes me feel better to say it, there’s no extra money that anybody gets for having designated a COVID death. That’s a common myth out there, but there’s no incentive whatsoever for any kind of healthcare institution to say, “I know they died of a gunshot wound, but they had COVID, so I’m going to count it as that.” Our chief medical examiner, as everywhere across the nation, always classifies deaths by the cause of death, not incidental findings.
Thank you, Dr. Piercey, for taking the time to answer our questions!
**********
For more health and beauty tips, click HERE.